 Kidney Stone
Kidney Stone
X-ray similar to mine
5/15/15
My husband Mike and I were sitting in a roomful of nurses, one of my favorite groups to be with. We were attending the lovely annual dinner that was sandwiched between two full days of meetings with the Maine State Nurses Association. I was so happy to be there. I basically dragged Mike along, but he was pretty happy when they served up a beautiful prime rib. Then during dessert, ZING…. flank pain…not bad yet, but there. I turned to Mike and said “I don’t know if I am getting a kidney stone or what!” We left shortly after that. We were camped in our travel trailer at Blackwoods Campground in beautiful Acadia National Park. The meetings were in Bar Harbor, Maine, the nicest setting I could imagine. Before getting stoned, we had enjoyed 2 gorgeous days of camping and touring around.
All night, I labored with the unrelenting horrid flank pain. The camper was cold..no electric hook ups there. No cell phone service either! Although our RV is 30 feet long, that little middle space wasn’t much of a place to pace with kidney stone pain, nausea, shakes, and clammy skin. In hindsight, I should have gone to the Bar Harbor ER. But, my first 2 kidney stones only caused me a single day of pain and eventually they passed on their own. I was being stoic and thinking, I can handle this on my own.
Not this time.
If I had gone to the ER that night, maybe I could have skipped the next several days of misery. I made a stupid choice.
5/16/15
We, or HE packed up our stuff and we drove home in the morning. I was loaded up with ibuprofen and so the pain wasn’t bad, but I felt like shit warmed over. I hated to miss the second day of meetings because a Facebook friend was going to speak about Patient Advocacy for Nurses. I got home and started drinking water like a camel. That night, the pain was back, in my back, in the black night. UGH. No doubt, I had to be seen by someone who knew more about kidney stones than I did.
5/17/15
Sunday we trooped off to St Joseph’s ER, where I got a cursory tap on both kidneys (this was my physical exam), a urinalysis and culture, antibiotics and 4 Oxycontin pills. Yup, you have blood and Nitrites in your urine Kathy. Advice, follow up with your primary care and a urologist and drink tons of liquids. mmmmhmmmm. No xray or CT scan done. I was actually ok with that until the next round of unrelenting pain. I am into Choosing Wisely, until wise choices are not made. In this case, they probably should have done at least an xray. This was partially my fault because I never want more tests or medicines than necessary.
This stone is different from my other ones.
5/18/15
Monday I crawled around my house thinking this bitch of a stone will pass. It HAS to. I’m feeling sick, constipated, and very miserable with pain. I have drunk gallons of water and strained the gallons of pee. Nothing.. And when old women are crabby AND constipated, they take Milk of Magnesia. No need to discuss this further because not everyone reading this will be a nurse or doctor.
5/19/15
I called St Joes for my urine culture results. Negative. I asked if I needed to take the rest of the Bactrim. She said “yes”, and “no further follow up needed”. Apparently she didn’t know about me, and my pain and my kidney stone. Then I called the urologist that the St Joes doctor recommended, thinking that I could skip right to the expert and avoid another visit with my Primary Care in between. They would not give me an appointment until I had blood work and a CT scan and I would have to get those ordered by my primary care doctor. My stone and I were being held hostage for more tests. Finally, I called my primary care doctor. They got me in within a few hours. He is my fave!! He got my history and ordered, not a CT, but an abdominal film and blood work. Then he gave me Flomax. It did help to reduce the pain, but it didn’t go away. I tossed and turned all night again with that stabbing constant pain. There was a pattern…when I wanted to lie down and sleep, that made the pain worse.
5/20/15
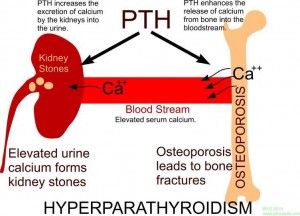
I called for my blood results and was told that my parathryoid hormone level was elevated but my blood calcium was not. How about the xray? (by biggest concern) No result on that yet, and the doctor is running 45 minutes late, and he might not get to it today, but we will let you know as soon as we get the reading….that’s what I was told. I waited all day long thinking maybe he would get to it, but they never got the reading of my xray from EMMC imaging that day, and in the busy-ness of the day, nobody called to get it. Another night of misery coming right up.
5/21/15
First thing in the morning I called the primary care office again. Before I got my question out, the med tech said, “I am going to call over there (EMMC) right now”. And so she did. I have a 1.5 cm or about a 3/4 inch kidney stone, one that will not pass on it’s own. The radiologist apparently did not think this was a significant clinical reading and didn’t share this information with my doctor after he read my film. I saw the xray myself, and I knew that the stone was at least 1cm….twice as big as my last one. I assumed because this stone was large, and would not pass on it’s own, that the reading and report out would be called to my doctor very quickly.
Now the fun really begins.
I really needed a urologist. My PC faxed a referral to a urologist we had discussed during my office visit. This was not the same one that St Joes recommended. When I spoke with that GU office these were their comments “We can’t give you an appointment until the doctor sees your lab and xrays. He is in surgery until this afternoon. I have to talk to my supervisor about this and she is out of town.” And then the kicker, “he only does procedures at Bar Harbor or Blue Hill Hospitals.” NO WAY am I circling back to Bar Harbor. I am too sick and miserable. And we have two hospitals right here in Bangor. So, my PC (primary care) called Urology Surgery, an affiliate of Eastern Maine Medical Center. At first they said I had to jump through the EMMC ER hoop (one of many so far)….I must go to the ER to get the urologist on call. OK, so now I am both sick and pissed off (get it?). I asked for the phone number and I called them myself. I firmly told them that I have a diagnosis..with X-rays, urinalysis and blood work to match, and I have visited an ER and my PC already. NO WAY am I going to add EMMC ER chaos, cost, and time to this. And I need to be taken care of. Guess what. That did it…I had to blow up just a little bit first, but I got into that office within 2 and half hours and I got the nicest, kindest, sweetest, most talented GU surgeon ever. He almost made me cry with gratitude. He knew I was sick by looking at me. My struggling kidney had already caused a rise in my creatinine level. By 5pm I was being wheeled into the EMMC OR for a ureteral stent placement, step one of two to rid myself of this stone. Everyone from the GU office, to the EMMC registration, to Patient intake, to preop, to OR to recovery room, anesthesia….all kind, caring and skilled. These are the names I remember..Courtney, Bev, Paula, Sue, and of course Jonas, my surgeon. They met my needs before I knew I had a need. Paula, my recovery nurse, helped me to the bathroom to pee for the first time after the procedure. She said…”you probably won’t pee yet, you just feel like you have to.” Her colleague said, “if she pees, Paula, you have to do a pee dance.” Paula did a pee dance..because, although it felt like I was passing glass…I peed!!! YAHOO
.
Lessons learned.
1. Don’t self diagnose. When your body is screaming at you with pain, pay attention. Do something about it right away.
2. Always bring an advocate, whenever and wherever you can. I am still unclear about how my stone will be removed, because I was so sick when I went to the Urologist’s office. I do remember something about lasers. It was a mistake not to bring Mike to the exam room with me. He is my trusted partner and extra pair of ears.
3. Don’t take no for an answer when you are getting dismissed, delayed or disregarded…and it won’t matter how good your people are…there is always some excuse or reason why your needs can’t or won’t be met when you need them met. Be persistent and advocate for yourself/your loved one.
4. Say thank you, frequently and sincerely. I thanked everyone over and over. I thanked my surgeon immediately when we very first met and we were shaking hands. I will write notes of thanks for the excellent care I received at EMMC and in the surgeon’s office.
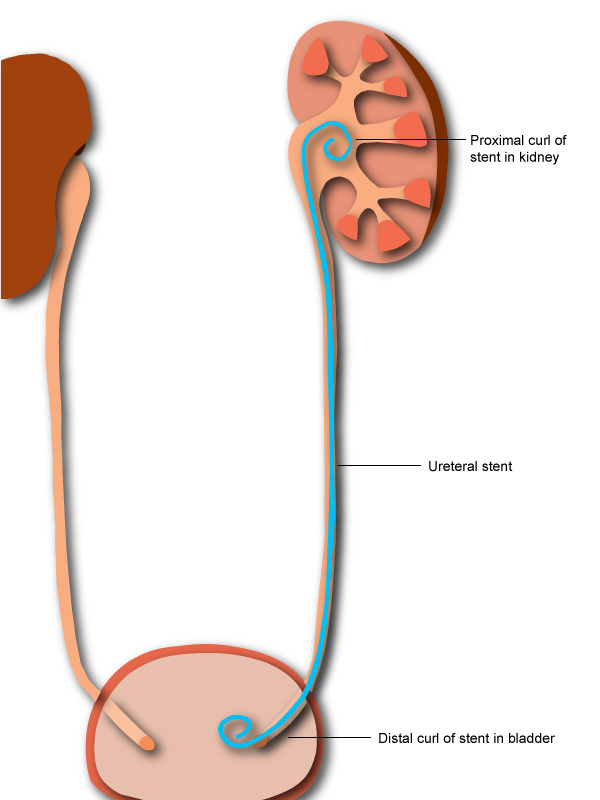
I am two days with my spanking new ureteral stent. This has allowed my brutalized left kidney to pass urine, despite my big stone. I am pain free. I have taken only 2 advil since my surgery. I am eternally grateful to my surgeon for pushing his scheduler to get me into surgery in 3 hours rather than in days. Her response to his request “are you kidding me?” She was obviously annoyed , but he didn’t back down. He was advocating for ME! She could steam about it all she wanted and she did, but she got me in.
I don’t share my story to get sympathy….I share it hoping to help patients to advocate for themselves and to be persistent when healthcare needs are not being met.
I also share in hopes that my caregivers, throughout this ordeal, will learn to simply do what’s right for their patients. Take care of them. Sick, miserable patients don’t want to hear excuses or be delayed. Patients want the right care, at the right time and in the right place.
My relief from pain and sickness came after almost a full week of battle, fighting for myself. I am still facing another GU procedure to remove the stone and the stent. Then maybe..just maybe… .a parathyroidectomy. I don’t anticipate any more battles, but my husband and I will be on alert and advocating for me.
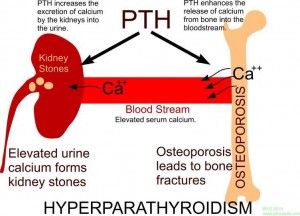
The reason I get kidney stones.

 Kidney Stone
Kidney Stone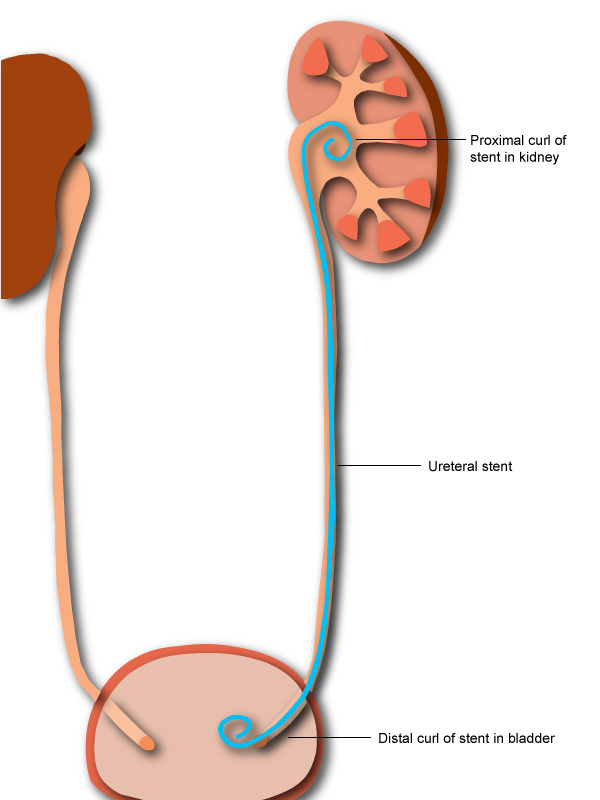
 I was up with the birds on April fools day this year, because I would attend my 4th annual MQC conference. I had things to do, people to see, experts to learn from, talks to hear and presentations to give. I had materials on Patient Safety to distribute (about 75 lbs of them in a very cumbersome wheeled bag), things to coordinate, and hugs to receive and give. My patient and supportive husband attends with me every year as well.
I was up with the birds on April fools day this year, because I would attend my 4th annual MQC conference. I had things to do, people to see, experts to learn from, talks to hear and presentations to give. I had materials on Patient Safety to distribute (about 75 lbs of them in a very cumbersome wheeled bag), things to coordinate, and hugs to receive and give. My patient and supportive husband attends with me every year as well. I don’t generally talk much about my own health, but when I think it might help somebody else out, why not? I have been a generally healthy fat woman most of my life, and I hardly ever go to the doctors. I don’t take many medicines and I haven’t had as much as a cold this winter. In my lifetime, I have had a two babies, a few gynecological procedures, got my tonsils out, had a broken ankle, two kidney stones, and that bout with uterine cancer a few years ago….quickly cured with surgery. That’s my history in a nutshell.
I don’t generally talk much about my own health, but when I think it might help somebody else out, why not? I have been a generally healthy fat woman most of my life, and I hardly ever go to the doctors. I don’t take many medicines and I haven’t had as much as a cold this winter. In my lifetime, I have had a two babies, a few gynecological procedures, got my tonsils out, had a broken ankle, two kidney stones, and that bout with uterine cancer a few years ago….quickly cured with surgery. That’s my history in a nutshell.



