Sepsis, a race against time
The day after my 83 year old father was readmitted to the Hospital, where he had contracted MRSA pneumonia, he slipped into Sepsis. He was extremely weak and feverish on admission, and they had put him through a lot of testing and diagnostics. My mother and I went into his room after lunch and I immediately saw a change in him. His skin was ashen, and he was hard to arouse. His nurse, a freshly minted RN, was typing on the computer on wheels right next to his bed. I asked her to check his vital signs. She said, “oh, he is just exhausted because of all the testing”. This was a reasonable excuse for his exhaustion, but I knew something was off. I reiterated that his color had changed and he wasn’t responding to us appropriately.
Dad’s nurse checked his blood pressure and it was dropping very rapidly. He was going into septic shock, part of sepsis. She called for the crisis team and they brought the code cart with them. While my mother and I watched, they injected life saving drugs and slowly brought Dad back. He was transferred into ICU and kept there for several days. Mum and I called the priest.
That was the most frightening day of my father’s illness. Neither he nor our family were ready for him to go, and so he fought valiantly to stay alive. His infection sapped his strength and he had become bedbound, but he lived for a few more months. Rapid response of the hospital team brought him back from the brink of death. Septic shock is a very dangerous medical condition. Dad’s sepsis symptoms were very subtle, and without my intimate knowledge of my father, and my ability to assess his status as a nurse, his sepsis might not have been caught as early as it was.
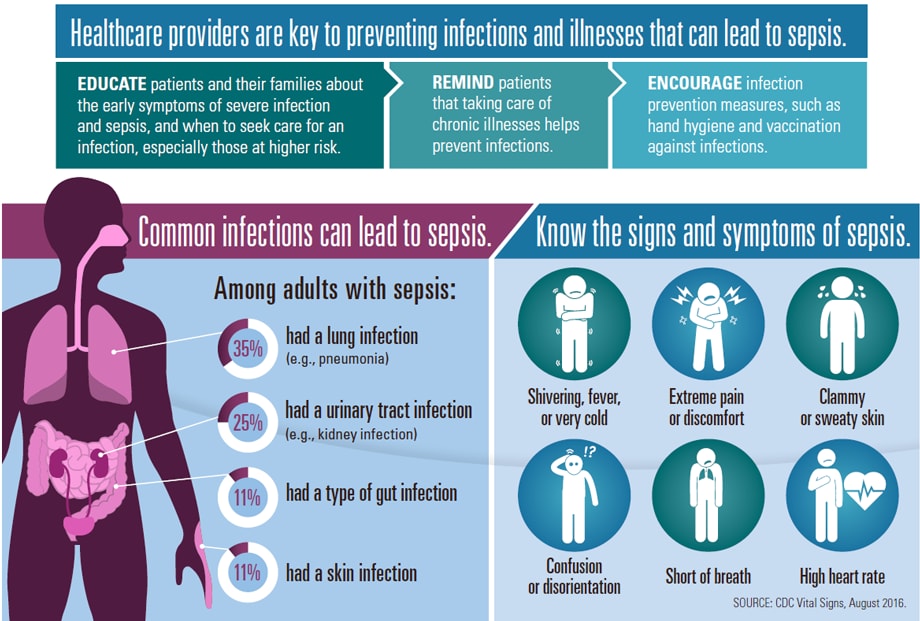
This week, the CDC has raised the alert about Sepsis and how important it is for everybody, not just medical people, to know the symptoms.
http://www.cdc.gov/vitalsigns/sepsis/index.html
Everyone should learn the signs of sepsis and be able to detect it in themselves or a loved on. Sepsis progresses rapidly and it can affect major organs and/or cause death. Rapid response to Sepsis is the only way to stop it. It is indeed a race against time.